Fill Your Tb Test Form
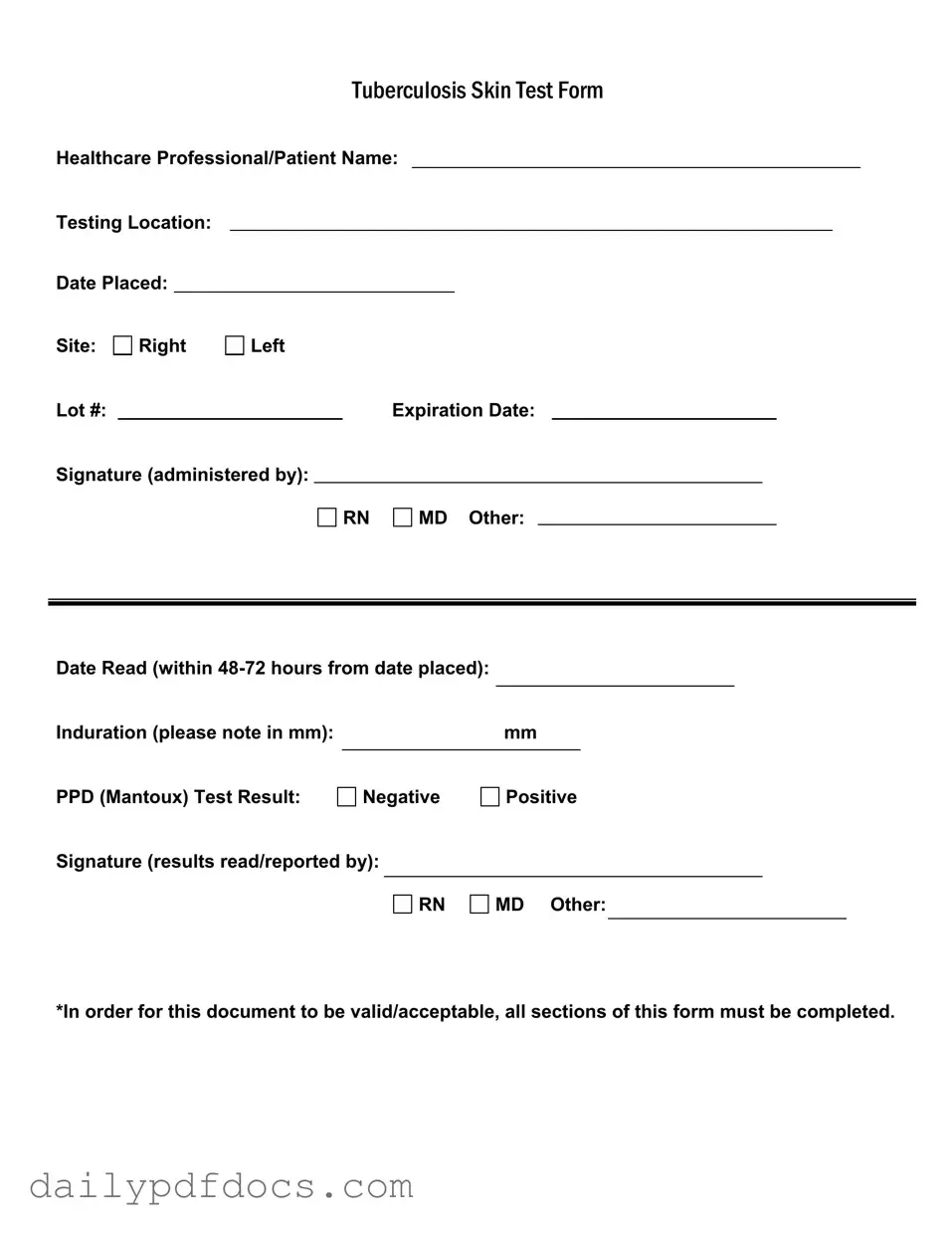
The Tuberculosis Skin Test Form is an essential document used in healthcare settings to track and record the administration and results of the PPD (Mantoux) test. This form includes critical information such as the names of both the healthcare professional and the patient, as well as the testing location and the date the test was placed. It also specifies the site of the test, whether on the right or left arm, and includes details like the lot number and expiration date of the test material. The form requires the signature of the administering professional, who may be a registered nurse, a medical doctor, or another qualified individual. After the test is placed, it must be read within 48 to 72 hours, and the results are documented, indicating whether the induration measured in millimeters is negative or positive. The signature of the professional who reads and reports the results is also required. For the document to be valid and acceptable, it is crucial that all sections are fully completed, ensuring accurate communication of the test's outcome.
Find Other Documents
How Do I Get My P45 - A secure method to handle the P45 form should be maintained for privacy and security.
Dd Form 2870 Download - The DD 2870 can help resolve disputes regarding medical treatment records.
Having a properly completed Motorcycle Bill of Sale is essential for both buyers and sellers in Minnesota, as it not only formalizes the sale but also helps in maintaining clear records. To ensure that you have everything you need for a smooth transaction, it is advisable to view the form and fill it out thoroughly, capturing all necessary details to protect your rights and comply with the law.
Employee Application - We encourage you to share any relevant skills that may benefit our team.
Common Questions
What is the purpose of the TB Test form?
The TB Test form is used to document the administration and results of the Tuberculosis (TB) skin test, also known as the PPD (Purified Protein Derivative) test. It ensures that all necessary information is recorded for accurate tracking and reporting of TB test results.
What information is required on the TB Test form?
All sections of the form must be completed. This includes the healthcare professional's name, testing location, date the test was placed, site of administration, lot number, expiration date, and the signatures of both the administrator and the individual reading the results. Additionally, the induration measurement and the test result (negative or positive) must be noted.
How soon should the TB test results be read?
The results of the TB test must be read within 48 to 72 hours after the test is placed. It is crucial to adhere to this timeframe to ensure accurate interpretation of the test results.
What does the induration measurement indicate?
Induration refers to the raised, hardened area at the site of the test. The measurement, noted in millimeters (mm), helps determine whether the test result is considered positive or negative. A larger induration typically indicates a positive result, suggesting possible exposure to TB.
What does a positive TB test result mean?
A positive TB test result indicates that the individual has been exposed to the bacteria that cause TB. However, it does not necessarily mean that the person has an active TB infection. Further evaluation and testing may be required to determine if the individual is infected or has latent TB.
What should I do if my TB test result is positive?
If your TB test result is positive, it is important to follow up with your healthcare provider. They may recommend additional tests, such as a chest X-ray or a sputum test, to assess whether you have an active TB infection and to discuss treatment options if necessary.
Can I use the TB Test form for any other purpose?
No, the TB Test form is specifically designed for documenting TB skin test results. It should not be used for other medical purposes or tests, as it contains specific fields relevant only to TB testing.
What happens if the TB Test form is incomplete?
If the form is incomplete, it may not be considered valid or acceptable. All sections must be filled out to ensure accurate documentation and reporting. Incomplete forms can lead to delays in processing and may require retesting.
Preview - Tb Test Form
|
|
|
|
|
TUBERCULOSISSKINTESTFORM |
||||||||
Healthcare Professional/Patient Name: |
|||||||||||||
Testing Location: |
|
|
|
|
|
|
|
|
|
|
|
||
Date Placed: |
|
|
|
|
|
|
|
|
|
|
|
|
|
Site: |
Right |
Left |
|
|
|
|
|
|
|
|
|||
Lot #: |
|
|
|
|
|
Expiration Date: |
|
|
|||||
Signature (administered by): |
|
|
|
|
|
|
|
|
|
||||
|
|
|
|
|
RN |
|
MD Other: |
|
|
|
|||
Date Read (within |
|
|
|
|
|
|
|
Induration (please note in mm): |
|
mm |
|
PPD (Mantoux) Test Result: |
|
|
|
Negative |
Positive |
||
Signature (results read/reported by):
RN
MD Other:
*In order for this document to be valid/acceptable, all sections of this form must be completed.
Similar forms
-
Vaccination Record: Similar to the TB Test form, a vaccination record documents the administration of vaccines, including details such as the healthcare provider, date administered, and type of vaccine. Both forms require signatures from healthcare professionals to validate the information provided.
-
California Residential Lease Agreement: A crucial document that outlines the terms of renting a property, ensuring clarity in vital areas such as rental payments and tenancy conditions. For more details, visit https://legalformspdf.com.
-
Medical History Form: This form collects comprehensive information about a patient's past medical conditions and treatments. Like the TB Test form, it often requires a healthcare professional's signature and is essential for accurate patient care.
-
Consent Form: A consent form is used to obtain a patient's permission for specific medical procedures or treatments. Both the consent form and the TB Test form must be signed by the patient and a healthcare provider, ensuring that all necessary information is documented.
-
Referral Form: A referral form is used when a healthcare provider recommends that a patient see a specialist. Similar to the TB Test form, it includes essential details such as patient information and the reason for the referral, requiring signatures for validation.
-
Patient Registration Form: This document collects basic information about a patient, including contact details and insurance information. Like the TB Test form, it must be completed thoroughly to ensure accurate patient records.
-
Lab Test Order Form: This form is used to request specific laboratory tests. It shares similarities with the TB Test form in that it includes patient details, the type of test being ordered, and must be signed by a healthcare provider.
-
Discharge Summary: A discharge summary provides a comprehensive overview of a patient's hospital stay, including treatments received and follow-up care instructions. Both documents require detailed information and signatures to ensure proper continuity of care.
-
Insurance Claim Form: This form is submitted to insurance companies for reimbursement of medical services. Like the TB Test form, it requires accurate information and signatures to be processed effectively.
Misconceptions
There are several misconceptions surrounding the Tuberculosis (TB) Test form that can lead to confusion. Understanding these misconceptions can help ensure that the testing process is smooth and effective.
- Misconception 1: The TB Test form can be partially completed.
- Misconception 2: The test result can be read after any time frame.
- Misconception 3: A negative result means no exposure to TB.
- Misconception 4: Only healthcare professionals can administer the test.
- Misconception 5: The lot number and expiration date are unimportant.
- Misconception 6: The form is not necessary for follow-up testing.
Some people believe that it is acceptable to leave sections of the form blank. However, to be valid, all sections must be completed.
It is a common misunderstanding that the test result can be read at any time. In reality, the result must be read within 48 to 72 hours from the date the test was placed.
A negative result indicates that the test did not show evidence of TB infection at that time, but it does not guarantee that a person has never been exposed to the bacteria.
While trained healthcare professionals, such as RNs and MDs, typically administer the test, other qualified individuals may also do so, provided they follow proper guidelines.
Some individuals may overlook the importance of the lot number and expiration date. These details are crucial for ensuring the test's validity and effectiveness.
There is a belief that the form is only needed for the initial test. In fact, it is important to maintain proper documentation for any follow-up tests as well.
File Attributes
| Fact Name | Description |
|---|---|
| Form Title | This form is officially titled "Tuberculosis Skin Test Form". |
| Healthcare Professional | The form requires the name of the healthcare professional administering the test. |
| Testing Location | The location where the test is administered must be specified. |
| Date Placed | The date when the test is administered must be recorded. |
| Induration Measurement | Induration must be measured in millimeters (mm) and noted on the form. |
| Test Result | The result of the PPD (Mantoux) test must be indicated as either negative or positive. |
| Signature Requirement | Signatures from healthcare professionals are required for both administration and result reporting. |
| Completion Requirement | All sections of the form must be completed for it to be valid and acceptable. |