Fill Your Annual Physical Examination Form
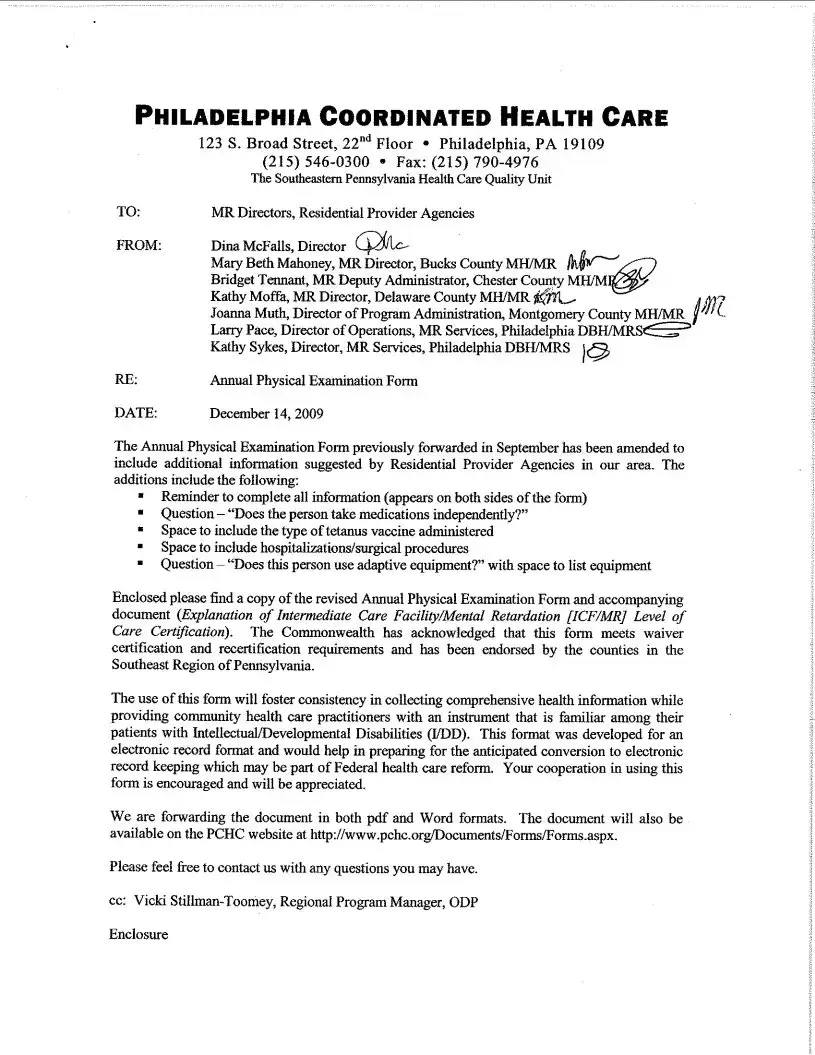
The Annual Physical Examination form serves as a crucial tool for both patients and healthcare providers, ensuring that comprehensive health assessments are conducted effectively. This form gathers essential information prior to a medical appointment, including personal details such as name, date of birth, and address, as well as a summary of medical history and current medications. It prompts individuals to disclose any significant health conditions, allergies, and immunizations, which are vital for accurate diagnosis and treatment. Additionally, the form includes sections for diagnostic tests, such as screenings for tuberculosis, mammograms, and prostate exams, providing a complete picture of the patient's health status. The general physical examination section captures vital signs and evaluates various body systems, facilitating thorough assessments. Recommendations for health maintenance and any necessary follow-up care are also documented, ensuring that patients receive tailored guidance based on their individual health needs. By completing this form, patients can help streamline their healthcare experience, ultimately leading to better health outcomes.
Find Other Documents
96 Well Plate Dimensions - Facilitates easy visual inspection of samples.
To facilitate a smooth transaction, it is vital for both buyers and sellers to familiarize themselves with the Minnesota Motor Vehicle Bill of Sale form, which serves as a legal record of ownership transfer. This document not only details the vehicle and sale price but also includes pertinent information about the involved parties, helping to ensure that everything is transparent and above board. For assistance in filling out the necessary paperwork, you can open the document and follow the guidance provided.
How to Travel With a Dog Internationally - Fill in your pet's date of birth accurately for identification purposes.
Common Questions
What is the purpose of the Annual Physical Examination form?
The Annual Physical Examination form is designed to gather essential information about a patient’s health before their medical appointment. This information helps healthcare providers assess medical history, current medications, allergies, and any significant health conditions. By completing this form, patients can facilitate a more efficient and thorough examination, reducing the need for follow-up visits.
Who should complete the Annual Physical Examination form?
Patients scheduled for an annual physical examination should complete this form. It is important that they provide accurate and comprehensive information. If a patient is a minor or requires assistance, a parent or guardian should fill out the form on their behalf. Additionally, any accompanying person can help ensure all sections are completed properly.
What information is required in Part One of the form?
Part One of the form requests personal details such as the patient’s name, date of birth, and address. It also asks for the Social Security Number, the name of the accompanying person, and a summary of any significant health conditions. Patients must list current medications, allergies, and immunization history, which are crucial for the healthcare provider to know before the examination.
How should current medications be listed on the form?
Patients should list their current medications in a structured format, including the medication name, dosage, frequency, diagnosis, prescribing physician, and the date the medication was prescribed. If there are many medications, patients are encouraged to attach a separate page to ensure all information is included. This helps the physician understand the patient’s medication regimen and any potential interactions.
What immunizations need to be reported on the form?
The form requires patients to report their immunization history, including Tetanus/Diphtheria, Hepatitis B, Influenza, and Pneumovax. Patients should indicate the dates of administration and the type of immunization received. Keeping this information updated is vital for the healthcare provider to assess the patient’s immunization status and recommend any necessary vaccinations.
What should I do if I have a history of communicable diseases?
If a patient has a history of communicable diseases, they must indicate this on the form. It is important to list specific precautions that should be taken to prevent spreading the disease to others. This information allows healthcare providers to take necessary measures during the examination and treatment, ensuring the safety of both the patient and others.
What kind of medical tests should be included in Part Two of the form?
Part Two of the form requires information about various medical tests, such as blood pressure readings, vision and hearing screenings, and any diagnostic tests like urinalysis or mammograms. Patients should provide results from recent tests, which can help the physician evaluate overall health and identify any areas needing further attention.
What happens if a patient has experienced a change in health status since the last examination?
If a patient has experienced a change in health status, they should indicate this on the form and specify the changes. This information is crucial for the healthcare provider to understand any new health concerns and adjust treatment plans accordingly. Open communication about health changes can significantly improve patient care.
Why is it important to complete the Annual Physical Examination form accurately?
Completing the form accurately is vital for ensuring that healthcare providers have a complete picture of a patient’s health. Inaccurate or incomplete information can lead to misdiagnosis, inappropriate treatment, or overlooked health issues. Patients are encouraged to take their time when filling out the form and to ask for assistance if needed.
Preview - Annual Physical Examination Form
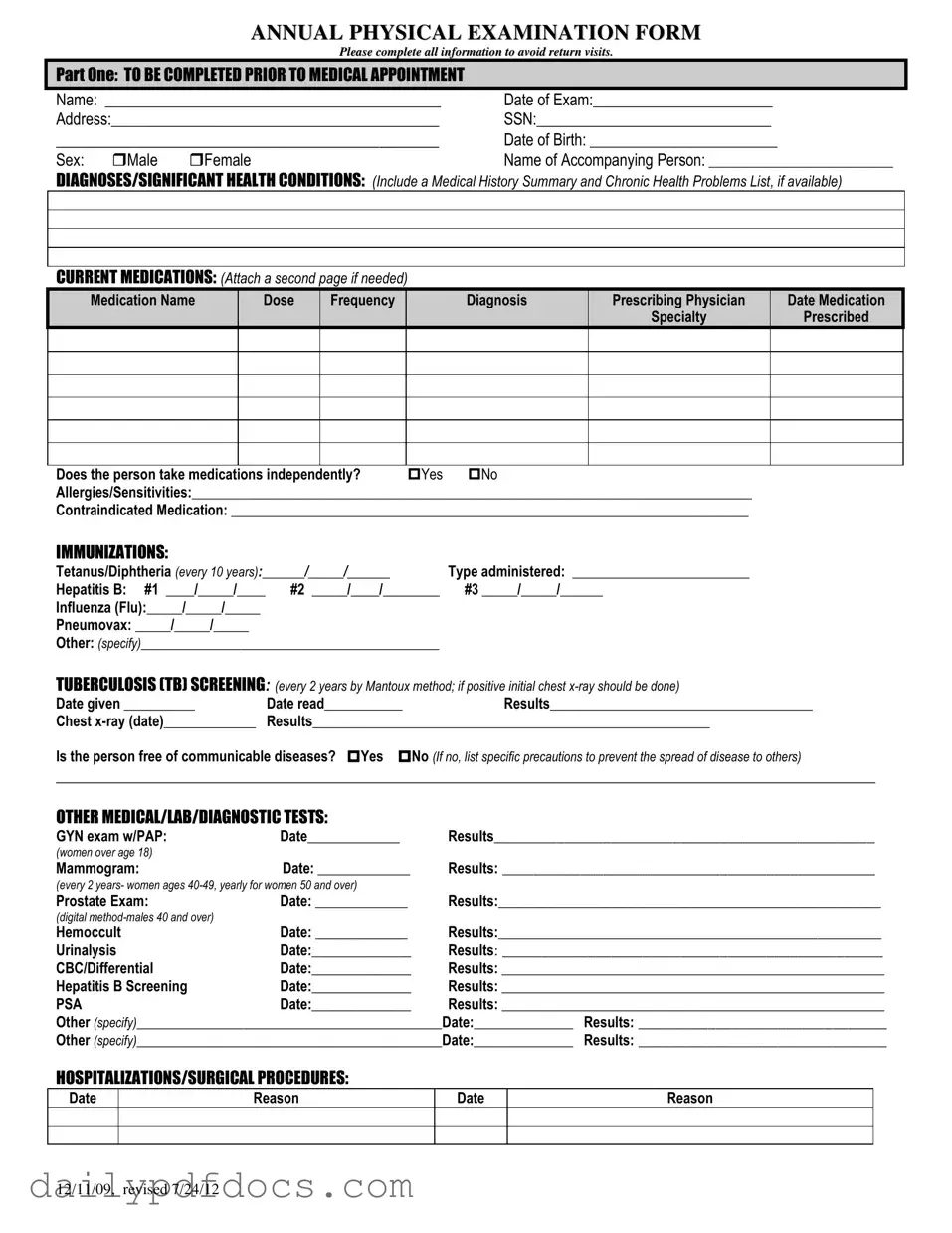
ANNUAL PHYSICAL EXAMINATION FORM
Please complete all information to avoid return visits.
PART ONE: TO BE COMPLETED PRIOR TO MEDICAL APPOINTMENT
Name: ___________________________________________ |
Date of Exam:_______________________ |
Address:__________________________________________ |
SSN:______________________________ |
_____________________________________________ |
Date of Birth: ________________________ |
||
Sex: |
Male |
Female |
Name of Accompanying Person: __________________________ |
DIAGNOSES/SIGNIFICANT HEALTH CONDITIONS: (Include a Medical History Summary and Chronic Health Problems List, if available)
CURRENT MEDICATIONS: (Attach a second page if needed)
Medication Name |
Dose |
Frequency |
Diagnosis |
Prescribing Physician |
Date Medication |
|
|
|
|
Specialty |
Prescribed |
Does the person take medications independently? |
Yes |
No |
Allergies/Sensitivities:_______________________________________________________________________________ |
||
Contraindicated Medication: _________________________________________________________________________
IMMUNIZATIONS:
Tetanus/Diphtheria (every 10 years):______/_____/______ |
Type administered: _________________________ |
|
Hepatitis B: #1 ____/_____/____ |
#2 _____/____/________ |
#3 _____/_____/______ |
Influenza (Flu):_____/_____/_____ |
|
|
Pneumovax: _____/_____/_____ |
|
|
Other: (specify)__________________________________________ |
|
|
TUBERCULOSIS (TB) SCREENING: (every 2 years by Mantoux method; if positive initial chest |
||
Date given __________ |
Date read___________ |
Results_____________________________________ |
Chest |
Results________________________________________________________ |
|
Is the person free of communicable diseases? Yes No (If no, list specific precautions to prevent the spread of disease to others)
_________________________________________________________________________________________________________
OTHER MEDICAL/LAB/DIAGNOSTIC TESTS:
GYN exam w/PAP: |
Date_____________ |
Results_________________________________________________ |
(women over age 18) |
|
|
Mammogram: |
Date: _____________ |
Results: ________________________________________________ |
(every 2 years- women ages
Prostate Exam: |
Date: _____________ |
Results:______________________________________________________ |
|
(digital |
|
|
|
Hemoccult |
Date: _____________ |
Results:______________________________________________________ |
|
Urinalysis |
Date:______________ |
Results: _________________________________________________ |
|
CBC/Differential |
Date:______________ |
Results: ______________________________________________________ |
|
Hepatitis B Screening |
Date:______________ |
Results: ______________________________________________________ |
|
PSA |
Date:______________ |
Results: ______________________________________________________ |
|
Other (specify)___________________________________________Date:______________ |
Results: ________________________________ |
||
Other (specify)___________________________________________Date:______________ |
Results: ________________________________ |
||
HOSPITALIZATIONS/SURGICAL PROCEDURES:
Date
Reason
Date
Reason
12/11/09, revised 7/24/12

PART TWO: GENERAL PHYSICAL EXAMINATION
|
|
|
|
|
Please complete all information to avoid return visits. |
|
|
|
|
|
Blood Pressure:______ /_______ Pulse:_________ |
Respirations:_________ Temp:_________ Height:_________ |
Weight:_________ |
||||
|
|
EVALUATION OF SYSTEMS |
|
|
|
|
||
|
|
|
|
|
|
|
||
|
|
System Name |
|
Normal Findings? |
Comments/Description |
|
||
|
|
Eyes |
|
Yes |
No |
|
|
|
|
|
Ears |
|
Yes |
No |
|
|
|
|
|
Nose |
|
Yes |
No |
|
|
|
|
|
Mouth/Throat |
|
Yes |
No |
|
|
|
|
|
Head/Face/Neck |
|
Yes |
No |
|
|
|
|
|
Breasts |
|
Yes |
No |
|
|
|
|
|
Lungs |
|
Yes |
No |
|
|
|
|
|
Cardiovascular |
|
Yes |
No |
|
|
|
|
|
Extremities |
|
Yes |
No |
|
|
|
|
|
Abdomen |
|
Yes |
No |
|
|
|
|
|
Gastrointestinal |
|
Yes |
No |
|
|
|
|
|
Musculoskeletal |
|
Yes |
No |
|
|
|
|
|
Integumentary |
|
Yes |
No |
|
|
|
|
|
Renal/Urinary |
|
Yes |
No |
|
|
|
|
|
Reproductive |
|
Yes |
No |
|
|
|
|
|
Lymphatic |
|
Yes |
No |
|
|
|
|
|
Endocrine |
|
Yes |
No |
|
|
|
|
|
Nervous System |
|
Yes |
No |
|
|
|
|
|
VISION SCREENING |
|
Yes |
No |
Is further evaluation recommended by specialist? |
Yes |
No |
|
|
HEARING SCREENING |
|
Yes |
No |
Is further evaluation recommended by specialist? |
Yes |
No |
|
|
ADDITIONAL COMMENTS: |
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
Medical history summary reviewed? |
Yes |
No |
|
|
||
Medication added, changed, or deleted: (from this appointment)__________________________________________________________
Special medication considerations or side effects: ________________________________________________________________
Recommendations for health maintenance: (include need for lab work at regular intervals, treatments, therapies, exercise, hygiene, weight control, etc.)
___________________________________________________________________________________________________________
Recommendations for manual breast exam or manual testicular exam: (include who will perform and frequency)____________________
___________________________________________________________________________________________________________
Recommended diet and special instructions: ____________________________________________________________________
Information pertinent to diagnosis and treatment in case of emergency:
___________________________________________________________________________________________________________
Limitations or restrictions for activities (including work day, lifting, standing, and bending): No Yes (specify)
___________________________________________________________________________________________________________ |
|||
Does this person use adaptive equipment? |
No |
Yes (specify):________________________________________________ |
|
Change in health status from previous year? No |
Yes (specify):_________________________________________________ |
||
This individual is recommended for ICF/ID level of care? (see attached explanation) Yes |
No |
||
Specialty consults recommended? No |
Yes (specify):_________________________________________________________ |
||
Seizure Disorder present? No Yes (specify type):__________________________________ Date of Last Seizure: ______________ |
|||
________________________________ |
_______________________________ |
_________________ |
|
Name of Physician (please print) |
Physician’s Signature |
|
Date |
Physician Address: _____________________________________________ |
Physician Phone Number: ____________________________ |
||
12/11/09, revised 7/24/12
Similar forms
- Health History Form: Similar to the Annual Physical Examination form, the Health History Form collects personal information, medical history, and current medications. It serves as a foundational document for healthcare providers to understand a patient's background and health needs.
- Medication Reconciliation Form: This document is used to review all medications a patient is currently taking. Like the Annual Physical Examination form, it ensures that healthcare providers have an accurate list of medications, which is crucial for safe prescribing and avoiding drug interactions.
- Employment Verification Form: This document confirms the employment status of individuals, similar to how the Annual Physical Examination form validates a patient's health status. For more information, you can visit legalformspdf.com/.
- Immunization Record: The Immunization Record tracks vaccinations received by an individual. It shares similarities with the Annual Physical Examination form by documenting immunization history and any required updates, ensuring that patients are protected against preventable diseases.
- Consent for Treatment Form: This form is used to obtain a patient's permission for medical procedures. It is similar in that it requires personal information and may include health history, ensuring that healthcare providers have the necessary details before proceeding with treatment.
- Referral Form: A Referral Form is used when a primary care physician refers a patient to a specialist. It often includes medical history and current health conditions, paralleling the Annual Physical Examination form in its purpose to provide comprehensive health information to another provider.
- Follow-Up Care Plan: This document outlines the recommendations for ongoing care after a medical appointment. Like the Annual Physical Examination form, it includes evaluations and suggestions for future health maintenance, ensuring continuity of care for the patient.
Misconceptions
Understanding the Annual Physical Examination form is essential for a smooth medical experience. However, several misconceptions can lead to confusion. Here are five common misunderstandings:
- It is only for sick people. Many believe that annual physical exams are only necessary for those who are unwell. In reality, these exams are crucial for everyone, regardless of current health status. They help in identifying potential health issues early.
- Completing the form is optional. Some think that filling out the Annual Physical Examination form is not mandatory. However, providing accurate and complete information is essential to ensure a thorough evaluation by the healthcare provider.
- All information must be perfect. There is a misconception that every detail on the form must be flawless. While accuracy is important, healthcare providers understand that some information may change or be unknown. It’s better to provide what you can than to leave sections blank.
- Immunizations are not necessary if you feel fine. Many individuals assume that if they are not experiencing any symptoms, they do not need to update their immunizations. However, staying current with vaccinations is vital for preventing diseases and maintaining overall health.
- Only the doctor needs to review the form. Some people believe that only the physician needs to read the completed form. In truth, the information is valuable for other healthcare staff as well, ensuring that everyone involved in your care has a comprehensive understanding of your health history.
By addressing these misconceptions, individuals can approach their annual physical examination with greater confidence and clarity. Proper preparation leads to better health outcomes.
File Attributes
| Fact Name | Description |
|---|---|
| Purpose | The Annual Physical Examination Form collects essential health information to facilitate a thorough medical evaluation. |
| Patient Information | Patients must provide personal details such as name, date of birth, and address prior to their medical appointment. |
| Medication Disclosure | Patients are required to list current medications, including dosage and prescribing physician, to ensure safe medical practices. |
| Immunization Records | The form includes sections for documenting immunizations, such as Tetanus and Influenza, essential for preventive care. |
| TB Screening | Patients must undergo tuberculosis screening every two years, with results recorded on the form. |
| System Evaluation | A general physical examination section assesses various body systems to identify any abnormalities or concerns. |
| Health Recommendations | Providers can document recommendations for health maintenance, including lifestyle changes and follow-up tests. |
| Legal Compliance | In some states, the use of this form may be governed by specific health care laws, including patient privacy regulations. |
| Signature Requirement | The form must be signed by a licensed physician, confirming the accuracy of the information and the examination conducted. |
| Record Keeping | Completed forms are typically retained in the patient’s medical record for future reference and continuity of care. |