Fill Your Advance Beneficiary Notice of Non-coverage Form
The Advance Beneficiary Notice of Non-coverage, commonly referred to as ABN, plays a crucial role in the healthcare landscape, particularly for Medicare beneficiaries. This form serves as a notification to patients when a healthcare provider believes that a service or item may not be covered by Medicare. By receiving an ABN, patients are informed that they may be responsible for payment if Medicare denies coverage. The form outlines the specific services in question, the reasons why they might not be covered, and provides beneficiaries with options regarding their care. It also includes a section for patients to acknowledge their understanding of the potential costs involved. Understanding the ABN is essential for beneficiaries to make informed decisions about their healthcare and financial responsibilities. It empowers patients by ensuring they are aware of their rights and options before receiving services that may not be reimbursed by Medicare.
Find Other Documents
Texas Temporary Tag - Issuance of a temporary tag is often quick and hassle-free.
Additionally, for those looking to streamline the transaction process, utilizing resources like Washington Templates can help ensure that all necessary details are accurately captured in the Motorcycle Bill of Sale form.
Roofing Inspection Report Template - Identify any new changes or penetrations made to the roof since the last inspection.
Common Questions
What is the Advance Beneficiary Notice of Non-coverage (ABN)?
The Advance Beneficiary Notice of Non-coverage, commonly referred to as the ABN, is a form used by healthcare providers in the United States. It informs Medicare beneficiaries that a particular service or item may not be covered by Medicare. The notice allows patients to make informed decisions regarding their care and potential costs.
When should I receive an ABN?
An ABN should be provided to you before receiving a service or item that your healthcare provider believes may not be covered by Medicare. This typically occurs when the provider has reason to believe that Medicare will deny payment for the service, either due to the nature of the service or because it is considered not medically necessary.
What should I do if I receive an ABN?
If you receive an ABN, review it carefully. The form will outline the service in question, the reason Medicare may not cover it, and your options. You can choose to proceed with the service and accept financial responsibility or decline the service. It is important to ask your provider any questions you may have about the notice.
What happens if I do not sign the ABN?
If you choose not to sign the ABN, the healthcare provider may not proceed with the service. In some cases, they may still provide the service, but you could be responsible for the full cost if Medicare denies coverage. Signing the ABN protects you from unexpected charges by acknowledging that you understand the potential financial responsibility.
Can I appeal a denial of coverage after receiving an ABN?
Is there a specific format for the ABN?
The ABN must follow a specific format as outlined by the Centers for Medicare & Medicaid Services (CMS). It includes sections for the patient's information, the service being provided, the reason for non-coverage, and the patient's signature. Providers are required to use the official ABN form to ensure compliance with Medicare regulations.
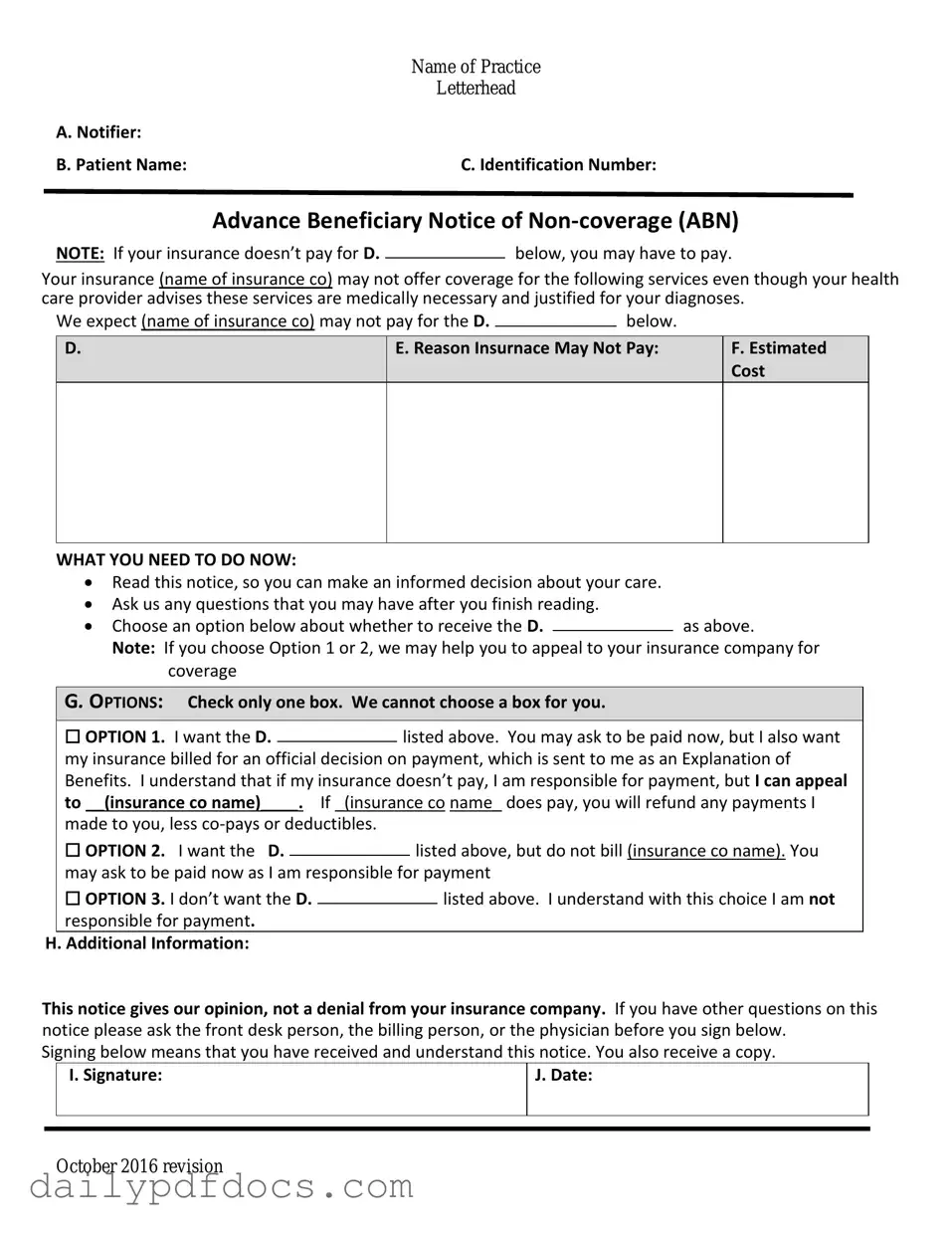
Preview - Advance Beneficiary Notice of Non-coverage Form
|
Name of Practice |
|
Letterhead |
A. Notifier: |
|
B. Patient Name: |
C. Identification Number: |
Advance Beneficiary Notice of
NOTE: If your insurance doesn’t pay for D.below, you may have to pay.
Your insurance (name of insurance co) may not offer coverage for the following services even though your health care provider advises these services are medically necessary and justified for your diagnoses.
We expect (name of insurance co) may not pay for the D. |
|
below. |
|
D.
E. Reason Insurnace May Not Pay:
F.Estimated Cost
WHAT YOU NEED TO DO NOW:
Read this notice, so you can make an informed decision about your care.
Ask us any questions that you may have after you finish reading.
Choose an option below about whether to receive the D.as above.
Note: If you choose Option 1 or 2, we may help you to appeal to your insurance company for coverage
G. OPTIONS: Check only one box. We cannot choose a box for you.
|
☐ OPTION 1. I want the D. |
|
listed above. You may ask to be paid now, but I also want |
||||
|
|
||||||
|
my insurance billed for an official decision on payment, which is sent to me as an Explanation of |
||||||
|
Benefits. I understand that if my insurance doesn’t pay, I am responsible for payment, but I can appeal |
||||||
|
to __(insurance co name)____. If _(insurance co name_ does pay, you will refund any payments I |
||||||
|
made to you, less |
|
|
|
|||
|
☐ OPTION 2. I want the D. |
|
|
listed above, but do not bill (insurance co name). You |
|||
|
|
|
|||||
|
may ask to be paid now as I am responsible for payment |
||||||
|
☐ OPTION 3. I don’t want the D. |
|
|
|
listed above. I understand with this choice I am not |
||
|
|
|
|
||||
|
responsible for payment. |
|
|
|
|||
H. Additional Information: |
|
|
|
||||
This notice gives our opinion, not a denial from your insurance company. If you have other questions on this notice please ask the front desk person, the billing person, or the physician before you sign below.
Signing below means that you have received and understand this notice. You also receive a copy.
|
I. Signature: |
J. Date: |
|
|
|
|
|
|
October 2016 revision
Similar forms
- Notice of Exclusion from Medicare Benefits (NEMB): This document informs beneficiaries that a specific service or item is not covered by Medicare. Like the Advance Beneficiary Notice of Non-coverage (ABN), it serves to clarify the financial responsibilities of the patient before the service is rendered.
- Medicare Summary Notice (MSN): This notice summarizes the services provided to a beneficiary during a specific period. It details what was billed to Medicare and what the beneficiary may owe, similar to the ABN, which outlines potential costs for non-covered services.
-
The Texas Mobile Home Bill of Sale ensures a clear transfer of ownership, outlining essential details such as buyer and seller information and specifications of the mobile home. For more information, visit https://mobilehomebillofsale.com/blank-texas-mobile-home-bill-of-sale.
- Patient Responsibility Notice: This document communicates to patients their financial obligations for services that are not covered by insurance. It parallels the ABN in that both documents aim to ensure patients understand their potential out-of-pocket costs before receiving care.
- Consent for Treatment Form: While primarily focused on obtaining permission for medical procedures, this form can also include information about costs and coverage. Like the ABN, it emphasizes the importance of patient awareness regarding financial implications associated with their care.
Misconceptions
The Advance Beneficiary Notice of Non-coverage (ABN) form is often misunderstood. Here are six common misconceptions about this important document:
- The ABN is only for Medicare patients. Many believe the ABN applies solely to Medicare beneficiaries. However, it can also be used in other situations where a provider anticipates that a service may not be covered by insurance.
- Signing an ABN means you must pay for the service. Some think that signing the ABN obligates them to pay for the service. In reality, it indicates that the provider believes the service may not be covered, and the patient has the option to accept or decline the service.
- The ABN is a guarantee of payment. Another misconception is that the ABN guarantees that the patient will be billed for the service. The form simply informs the patient of potential non-coverage; it does not guarantee payment.
- Providers must issue an ABN for all services. It is not necessary for providers to issue an ABN for every service. They are required to issue it only when they believe a service may not be covered.
- Patients cannot appeal if they receive an ABN. Some individuals think that signing an ABN prevents them from appealing a denial of coverage. In fact, patients still have the right to appeal decisions regarding coverage, even after signing the form.
- The ABN is only for specific types of services. There is a belief that the ABN applies only to certain services, such as elective procedures. However, it can be used for any service that may not be covered, regardless of its nature.
Understanding these misconceptions can help patients navigate their healthcare options more effectively and make informed decisions about their care.
File Attributes
| Fact Name | Description |
|---|---|
| Purpose | The Advance Beneficiary Notice of Non-coverage (ABN) informs Medicare beneficiaries that a service may not be covered. |
| When to Use | Providers must issue an ABN when they believe that Medicare will not pay for a specific service or item. |
| Beneficiary Rights | Patients have the right to refuse the service after receiving the ABN and can choose to pay out-of-pocket. |
| State-Specific Forms | Some states may have their own versions of the ABN, governed by state healthcare laws. |
| Signature Requirement | The ABN must be signed by the beneficiary or their representative to acknowledge understanding of the potential non-coverage. |
| Validity Period | The ABN is valid only for the specific service or item listed and for the date indicated on the form. |
| Consequences of Not Using | If an ABN is not provided when necessary, providers may not be able to collect payment from the patient for non-covered services. |